Chief of the department: Bruslik Sergey Vladimirovich, M.D., Ph.D.
As part of the Pirogov National Medical and Surgical Center the department of ultrasound and
To date, the Pirogov National Medical and Surgical Center has performed more than 600 ultrasound ablations in 380 patients, which allows the institution to take the leading position in Russia and Europe in terms of the number of treated patients with ultrasound ablation.
The main activities of the department:
- Ultrasound diagnosis (preparation for ultrasound)
- HIFU (ultrasonic ablation)
- Minimally invasive surgery
In the Pirogov National Medical and Surgical Center the whole spectrum of ultrasound studies is performed for outpatients by highly qualified specialists
Contact Information
Address: 105203, Moscow, Nizhnyaya Pervomayskaya str., 70
Contact phone number:
Fax:
How to reach us by using public transport
“Pervomaiskaya” metro station (last carriage of the train out of the city centre). From “Pervomaiskaya” metro station by any tram or trolley bus go to the stop “15th Parkovaya Street”. Go along the 15th Park Street to the intersection with the Nizhnyaya Pervomaiskaya Street, turn left and walk about a hundred meters to the entrance of the Pirogov National Medical and Surgical Center.
Ultrasound diagnostics
The special value of the method is high diagnostic value and economic attractiveness. Modern digital equipment has a high resolution. On equipment of the department — modern ultrasonic devices of expert class. This provides accurate diagnostics.
We conduct a comprehensive ultrasound examination:
- organs of the abdominal cavity, including examination of the liver, gallbladder and bile ducts, spleen, kidneys, adrenals, retroperitoneal space;
- urinary system;
- organs of small pelvis, scrotum;
- thyroid gland, mammary glands, salivary glands, lymph nodes;
- soft tissues;
- vessels by the method of dopplerography.
The department performs minimally invasive interventions under the supervision of the US. These are diagnostic and therapeutic punctures, the installation of drains, sclerosing cysts and other formations.
Your choice will be correct if you contact our Center.
Preparation for ultrasound of the abdominal cavity organs
Examination of the abdominal cavity is performed on an empty stomach. Before the examination should be at least
2 days before the ultrasound, if necessary, the doctor can prescribe espumizan or activated charcoal — 2 tablets 3 times a day, before each meal, or another drug.
Preparation for ultrasound of the gallbladder to determine its contractile function
The study is performed on an empty stomach (see preparation for ultrasound of the abdominal cavity), for the study to have a cholagogue breakfast.
Cholagogue breakfast can consist of:
- 250 ml of fatty cream or sour cream (fat content of at least 25%);
- the same amount of cottage cheese;
- a few pieces of bitter chocolate and a banana.
Preparation for ultrasound of the bladder, prostate
When transrectal examination of the prostate follows: three days before the procedure to exclude from the diet products that cause gas formation; eve dinner light meals.
In the case of ultrasound transabdominal method: for two days, exclude the use of gas-producing products; fill the bladder — drink an hour before the procedure 1 liter of water; The study is possible only with a filled bladder.
In the study of the bladder — drink an hour before the procedure, 1 liter of water (the study is possible only with a filled bladder).
Preparation for ultrasound of pelvic organs in women
The study is performed in a planned manner on the 5th-7th day of the menstrual cycle.
By transvaginal study no preparation is required.
In the case of ultrasound transabdominal method: for two days, exclude the use of gas-producing products; fill the bladder — drink an hour before the procedure 1 liter of water; The study is possible only with a filled bladder.
Preparation for ultrasound of mammary glands in women
The study is performed in a planned manner on the 5-10th day of the menstrual cycle.
Preparation for ultrasound of the kidneys, thyroid gland, salivary glands, scrotum organs is not required.
HIFU (ultrasonic ablation)
The modern level of development of medicine dictates new requirements: all aspirations of specialists are aimed at developing radical methods of treating tumors with the least traumatism and good tolerance of patients. HIFU technology (high energy focused ultrasound treatment or ultrasonic ablation) best meets these requirements.
Ultrasound ablation (HIFU) is the most modern non-invasive (remote) method of local destruction of formations in the world.
Today this is the only non-invasive method of destruction of the tumor focus, the treatment is carried out without disrupting the integrity of the skin.
The only ultrasound system in Russia “JC” (HIFU), available to a wide range of patients, is in the Pirogov National Medical and Surgical Center.
The principle of high-intensity focused ultrasound is based on the ability of an ultrasonic wave to penetrate through tissues without damaging them. At the point of focusing of waves created with a special lens, there is an increase in temperature sufficient for the development of necrosis (lesion focus) of pathological formation.
Subsequently, the focus affected by focused ultrasonic waves (HIFU) is gradually wrinkled and replaced by a fibrous tissue, a scar is formed.
For the first time using high-energy ultrasound instead of a surgeon’s scalpel for the destruction of tumor tissue, specialists of the University of Illinois began in the forties of the last century. Since 1997, since the appearance of the first industrial installations, the world practice has more than 100 000 patients treated with this method with tumors of the liver, kidneys, mammary glands, prostate gland, fibroids of the uterus.
Advantages of HIFU are: organ-preserving intervention; short terms of rehabilitation (there is no need for active infusion therapy, treatment is remotely, there is no need for a long stay in the hospital).
In comparison with currently available invasive ablation methods, this method does not require the addition of special conductors (electrodes for radiofrequency ablation, light-conducting fibers for laser ablation, a special hollow needle for cryoablation with liquid argon) to the tumor tissue.
The method of ultrasonic ablation is indicated in the treatment of benign and malignant tumors of various localizations (liver, pancreas, kidneys, mammary gland, etc.), except for lesions of the brain, lungs, intestines, bones of the skull and spinal column.
The results of the clinical application of ultrasonic ablation are very encouraging for oncologists, surgeons, gynecologists and, most likely, the method will soon take a worthy place in the treatment of cancer.
The uniqueness of HIFU technology lies in the fact that the philosophy of the progressive development of medical care is manifested in it: from traditional interventions to minimally invasive and, now, to non-invasive.
To date, we have performed about 400 ultrasound ablations for tumors of various locations, which is 1/3 of the total European experience in this field of medicine.
In the Pirogov National Medical and Surgical Center we perform remote ultrasound ablation of liver formations on the apparatus of JC (manufacturer: Chongqing Haifu (HIFU) Technology Co., Ltd.).
Ultrasonic ablation in liver tumors
Indications
- Primary solid liver tumors (adenomas, hemangiomas, hepatocarcinomas)
- Secondary liver damage (as a cytoreductive therapy)
Advantages of technology (HIFU)
- Non-invasiveness
- Absence of dependence on the size and histological structure of the tumor
- Safety of treatment with close proximity of the tumor to large vessels of the liver, inferior vena cava, aorta
- The possibility of affecting the maximum number of tumors with multiple lesions
- Compatibility of ultrasound ablation with systemic polychemotherapy
- The possibility of rapid rehabilitation
- If necessary — treatment in several stages with an interval of 7 days and repeated exposure to previously treated foci
Contraindications
- Diffuse hepatocarcinoma or disseminated metastatic process
- Cirrhosis of class C liver (Child-Pugh)
- Thrombosis of the portal vein
- Thrombocytopenia <50?103L
- Coagulopathies (PTI less than 40%, INR more than 1.5, APTT more than 45 sec)
- Rough scar changes of the skin
- Severe patients with multiple organ dysfunction
The list of necessary analyzes and pre-surgery (HIFU)
- Blood and urine tests
- Blood group and Rh factor
- General blood analysis
- Biochemical blood test (advanced)
- Coagulogram
- Markers of hepatitis, HIV, Wasserman’s reaction (syphilis)
- Oncomarkers (AFP, REA, CA
19-9, CA 125, CA15-3, etc.) - Clinical analysis of urine
X-ray examination of the chest organs or, if necessary, CT of the chest (with previously detected metastases)- External respiration function
- ECG
- Ultrasound of the abdominal cavity organs
- CT of abdominal organs with intravenous contrast
- Biopsy of liver foci
Conditions for carrying out HIFU — ablation
To perform the procedure, patients are hospitalized in a hospital. Treatment is performed under conditions of general anesthesia with controlled respiration. During treatment, due to short ultrasonic pulses, the tissue of the node is heated with subsequent coagulation necrosis. The treatment process is carried out under ultrasound in real time. The time of therapeutic manipulation depends on the size and number of nodes.
Clinical observation
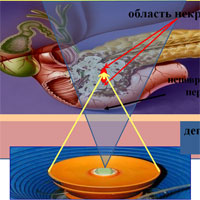
Computed tomography of abdominal organs with intravenous contrast:
 Fig. 3a. Tumor of the right lobe of the liver, 4.5 cm in diameter (two arrows). |
 Fig. 3b. After performing ultrasound ablation (own observation), the ablation volume is 93% (arrow). |
Ultrasonic ablation in uterine myomas
Indications
- Women of reproductive age who want to save the uterus and plan a pregnancy
- Women in premenopausal or menopause who want to keep the uterus
Advantages of technology (HIFU)
- Non-invasiveness
- Organ-preserving intervention
- Preservation of genital function
- High efficiency for large uterine myomas
- Effects on the maximum number of nodes in multiple lesions
- Absence of blood loss
- Node regression for
6-9 months - Rapid disappearance of clinical manifestations of uterine fibroids
- Absence of growth of treated nodes and relapses in the long-term period
- Good cosmetic effect
- Short terms of rehabilitation
- With HIFU, there is no need to subsequently find patients in intensive care units, treatment is remotely, there is no need for a long stay in the hospital
Contraindications
- Obesity
3-4 st. - Rough scar changes of the skin
- Hyperplastic processes in the endometrium
- Temporary contraindications may include infectious diseases of the pelvic organs, intrauterine contraceptives
The list of necessary analyzes and pre-surgery (HIFU)
- Blood and urine tests
- Blood group and Rh factor
- General blood analysis
- Blood chemistry
- Markers of hepatitis, HIV, Wasserman’s reaction (syphilis)
- Clinical analysis of urine
- Gynecological examination
- Visit the gynecologist
- Ultrasound (transabdominal and transvaginal)
- Smears
- Separate diagnostic curettage
- Chest
X-ray examination - ECG
- Magnetic resonance imaging with contrasting of organs of the pelvis
Conditions for HIFU-ablation
To perform the procedure, the patient is hospitalized for
The treatment process is carried out under ultrasound in real time. The time of therapeutic manipulation depends on the size and number of nodes and on average takes from 3 to 6 hours. During the procedure, the patient lies on her stomach. The patient does not experience pain, there may be a feeling of warmth and sensations similar to those experienced by a woman during menstruation.
Patients can return to their normal professional activities the day after the treatment. The technology of HIFU ablation is a method that will allow a significant part of women suffering from clinical manifestations of uterine myoma quickly, without disrupting personal and professional plans, to cure anemic uterine bleeding, dysuric disorders and intimate problems.
As a rule, treatment is carried out in one stage. To monitor the effectiveness of the procedure after 2 weeks, an MRI with contrast is performed. According to the world literature, in 79.3% of women the clinical manifestations of uterine myoma decreased after 6 months. When ablation of large nodes (up to 9 cm) after 6 months, a decrease in volume was observed, on average by 56%.
Clinical observation
MRI of pelvic organs:
 Fig. 4a. Myomatous node along the front wall, dimensions 75x83mm (two arrows). |
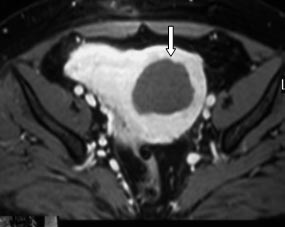 Fig. 4b. After performing ultrasonic ablation (own observation), the ablation amount is 89% (arrow). |
Minimally invasive surgery
Doctors of the department have a vast experience of minimally invasive interventions in various diseases. A special feature of the team is that ultrasound specialists, radiologists, and surgeons are assembled in one team, this allows performing a wide range of interventions from diagnostic (puncture, biopsy) to therapeutic (drainage, sclerotherapy, bile excretion). In addition, specialists of this department perform ultrasound ablation. All this allows to carry out complex, stage-by-stage, multicomponent treatment.
The list of minimally invasive surgical interventions:
- Percutaneous, transvaginal and transrectal therapeutic and diagnostic punctures of the cavity and duct structures of the abdominal cavity, retroperitoneal space, small pelvis, superficial organs and soft tissues under the supervision of ultrasound and RTV
- Percutaneous external drainage of the abdominal cavity, pleural cavities and pericardial cavity under the control of ultrasound and RTV
- Percutaneous external drainage of cavities (cysts and abscesses) of the abdominal cavity, retroperitoneal space and pelvic cavity under the control of ultrasound and RTV
- Percutaneous transhepatic echinococcectomy, echinococcectomy from the spleen and kidneys under the control of ultrasound and RTV
- Drainage of adrenal cysts under ultrasound and RTV control
- Percutaneous extra-gastric cystogastrostomy under the supervision of ultrasound and RTV
- Percutaneous transhepatic cholecystostomy under the control of ultrasound and RTV
- Percutaneous transhepatic external and external-internal biliary excretion (cholangiostomy) under the supervision of ultrasound and RTV
- Percutaneous transhepatic endoprosthetics of choledochia under the control of RTV
- Percutaneous ablation (alcoholization) of liver formations under the supervision of ultrasound
- Providing access to portal embolization (chemoembolization) of liver formations under the supervision of ultrasound
- Puncture and drainage of kidney cysts under ultrasound guidance
- Percutaneous nephrostomy under ultrasound guidance
- FNAB of bulk formations of the thyroid gland, mammary glands, soft tissues under ultrasound control
- FNAB volumetric formations of the abdominal cavity organs, retroperitoneal space and pelvic cavity under ultrasound control