Chief of the department: Jojua Alhas Valterovich, Ph.D, doctor of highest category, associate professor.
The department was formed around a group of highly qualified doctors, specializing in different branches of traumatology and orthopedics in 2011, what allowed us to treat every single musculoskeletal system disease.
Our specialists are constantly increasing their qualification via sharing professional experience with both Russian and foreign leading traumatologists-orthopedists, taking part in annual scientific conferences and working on probation in leading medical centers, including foreign ones.
The department works in scheduled or emergency regime 24 hours a day and conducts approximately 10 operations a day (around 2500 a year) among with outpatient consultations.
The operations are conducted within the hi-tech health care state programs and compulsory medical insurance. We also cooperate with the majority of Russian voluntary health insurance companies and offer a number of pay medical services.
What do we treat?
Deforming arthrosis of larger joints
Сoxarthrosis — the arthrosis of a hip joint.
The damaged, “worn out” joint (in this particular case, all of it, including femoral head and acetabulum) would be replaced with an artificial one during the operation.
The traumatologist would pick the needed implant model depending on the stage and dynamics pace of the disease.
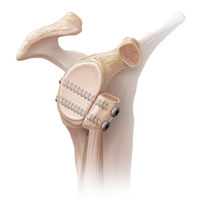
Gonarthrosis — the arthrosis of a knee joint. Treating includes the replacement of all the joint components: femoral, tibial and the meniscus (high-molecular polyethylene gasket) between them.
Omarthrosis — the arthrosis of a shoulder joint. The damaged, “worn out” joint components are replaced. In case the disease is followed by unrecoverable rotator cuff tendon tear, the reversal joint endoprosthesis replacement becomes an option.
Endoprothesis replacement is also conducted in order to cure elbow, talocrural and foot joints diseases.
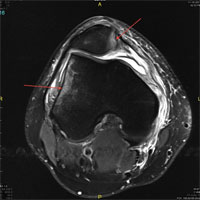
Knee instability
Our department doctors have an immense experience in operating an unstable knee.
Both synthetic (biodegradable) and patients’ own materials are used during the ligamentous apparatus surgery.
The individual approach to every single patient, considering his level of physical activity and sport advancement, all the modern equipment and the stationary rehabilitation allow our patients to return to their normal physical and every-day activities routine.
Operative treatment of the patella instability
The primary patellar dislocation is usually treated conservatively but requires a competent rehabilitation period conduction.
In case the patella dislocation is recurrent, the operative treatment becomes necessary. In order to discover the true reasons of the disease (the inborn joint peculiarities) a number of medical examination procedures are conducted, including radiography, CT and magnetic resonance imaging procedure. It would help the doctor to work out the further strategy and to pick an adequate type of an operative treatment.
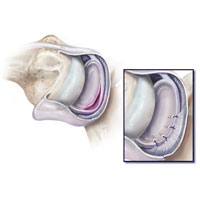
Arthroscopic suture of knee joint meniscuses
Meniscus tear can be treated by stitching it, using a special suture material, preserving the biomechanical function and preventing the further gonarthrosis progression.
In case the tear is chronic and degenerative, partial resection is performed using modern technologies such as cold plasma ablation.
Fracture osteosynthesis of varied localizations and complexities
Osteosynthesis, conducted via mini-invasive access, allows reducing pain syndrome during the postoperative period, to accelerate soft tissues and bone stock regeneration and to lower the possibility of postoperative complications (fracture site inflammation and suppuration).
Stable osteosynthesis with the use of angular stability plates and locking nails, conducted in our center, ensures reliable fragments fixation. This stands in a good stead for patients’ activation during the early postoperative period and shortens the inpatient and disability periods.
Shoulder joint instability treatment
Primary shoulder joint dislocation (after correction) is usually treated conservatively: up to 4 weeks immobilization period followed by a course of exercise therapy.
The shoulder joint stabilization is indicated in case of the dislocations repentance.
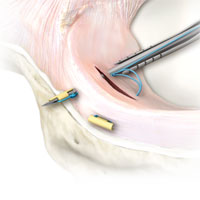
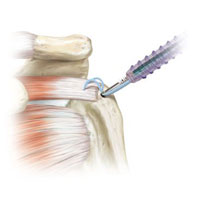
Soft-tissue shoulder joint stabilization (Bankart’s operation): damaged intraarticular structures, such as the articular lip with the capsule and ligaments, are moved and fixed to their anatomical attachment site using biodegradable anchoring fixators. The operation is conducted by arthroscopic, mini-invasive method.
Repeated shoulder joint dislocations cause humeral head and articular scapula process bone defects. In this case, Latarje operation with the transposition of the coracoid process is necessary to fill the deficiency of the articular surfaces. It allows making away with the risk of subsequent dislocations.
Arthroscopic suture of rotator cuff tendons
The rotator cuff is a complex of four muscles’ tendons, attached to the humeral head, which participate in the shoulder joint basic movements. If various ruptures and detachments cause painful limitation of movements in the shoulder joint (progressing up to a pseudoparalysis) they will be moved and fixed to the humerus using anchoring fixators.
Adhesive capsulitis (“frozen shoulder”) treatment
If the conservative treatment of an adhesive capsulitis is ineffective, we recourse to operative treatment (arthroscopic excision of a rigid inflamed joint capsule). It’s essential to conduct early patient activation among with the onset of exercise therapy in order to prevent the capsulitis re-development. Concerning this, a microcatheter is inserted into the joint cavity to at the end of the operation and, thus, anesthetics are injected in the early postoperative period. This allows our patients to start exercise therapy in several hours after the operation.
Clavicle instability (dislocation)
Acromial extremity of clavicle dislocation, as the most common pathology, is accompanied by tear of ligaments between the clavicle and scapula and the coracoid process. Depending on the injury duration and the clavicle dislocation stage, a number of successfully applied in practice techniques are used.
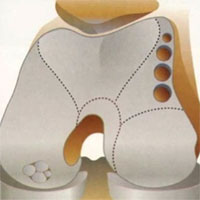
Hallux valgus — valgus deformation of the first toe/“foot bonelet”
The disease is described as an excessive bone tissue overgrowth around the I foot metatarsophalangeal joint.
Initial stages of the disease cause edema and pain in the joint area. Later, along with the disease dynamics, the foot deformation and pain enhance and it becomes challenging to pick a fitting pair of shoes.
In this case, we use an operative method of treatment, so-called “corrective osteotomy”. It is conducted not only to remove bone growths (“cones”), but also to correct the axis and the altered foot arch formation.
Chevron osteotomy, Scarf osteotomy and hammer toe correction — a complex operation aimed at restoring the foot support function.
Articular cartilage pathology treatment
There is a possibility to conduct operative treatment, aimed at restoring articular cartilage focal defects, such as:
Mosaic chondroplasty. The bone-cartilaginous fragment of the affected joint site is replaced by a healthy one, taken from an unloaded joint zone.
Collagen membrane implantation into the cartilage defect zone via matrix-induced autohondrogenesis technique
Microfracturing is a method of treating small articular cartilage defects. Small holes in the subchondral bone are made in order to form a blood clot (which would later form a fibrocartilage) in the defect area and to release growth factors.
Hip joint arthroscopy
Hip arthroscopy is an extremely effective way of treating pathologies, which inevitably lead to the coxarthrosis progression. The joint lip damage and femur-acetabulum impingement are the most common pathologies.
Joint replacement can be avoided if these pathologies are detected on early stages and eliminated by joint lip arthroscopic suture or hip joint arthroscopic arthroplasty.
Elbow joint arthroscopy
Arthroscopy is widely used for treating epicondylitis, elbow joint contracture, chondromus bodies removal and synovial ligament syndrome.
Distal biceps tendon detachment
The main function of the biceps muscle of arm is the upper limb flexion (in the elbow joint) and supination of the forearm (turning the palm upward).
The majority of tendon detachments occurs while lifting a heavy object in everyday life or while doing sports (weight lifting, for instance). Men aged over 40 years form a particular group that requires special attention.
It is necessary to resort to operative treatment in order to restore the injured upper limb and to eliminate the deformation.
There are several surgical techniques. The main principle is to move and fix the distal biceps tendon to the site of its anatomical attachment to the radial bone:
- Anatomic fixation
- Direct access fixation
The fundamental difference between these techniques is picking the location of the attachment to the radial bone.
The anatomic technique includes tendon fixation to the radial tuberosity by additional access. Thus, both elbow joint flexion and supination are restored.
Patients with Dupuytren’s contracture treatment
Factors, which affect the Dupuytren’s contracture progression can be either traumatic, genetic, or caused by a metabolic disorder.
Hands are affected in the first place. Finger movement restriction is developed and the patient’s life quality decreases.
Conservative treatment, along with needle aponeurotomy (a technique of finger mobility restoration without a single cut), is conducted in the early stages.
In far-reaching cases we resort to operative treatment (healing tissue excision).
Carpal tunnel syndrome treatment
Carpal tunnel syndrome is a neurological disease that causes prolonged pain and finger numbness.
The disease progression occurs due to the compression of median nerve and surrounding carpal canal tendons.
If the conservative treatment (which includes complex anti-inflammatory therapy) is ineffective, median nerve neurolysis is conducted. In this case, transverse carpal ligament is dissected, relieving median nerve compression.
Department doctors
 |
Alhas Valterovich Jojua
The department chief, candidate of medical sciences, traumatologist-orthopedist of higher category, associate rrofessor
|
 |
Kirill Evgenyevich Baranov
Traumatologist-orthopedist
|
 |
Mihail Arturovich Bolotnikov
Traumatologist-orthopedist
|
 |
Mihail Olegovich Vihtar
Traumatologist-orthopedist
|
 |
Oleg Andreevich Goryachev
Traumatologist-orthopedist
|
 |
Andrey Mihaylovich Denisov
Traumatologist-orthopedist
|
 |
Alexander Nikolayevich Kobilchenko
Traumatologist-orthopedist
|
 |
Peter Dmitrievich Kuzmin
The Head of the Traumatology-Orthopedics course (the Department of Surgery), traumatologist-orthopedist
|
 |
Oleg Nikolaevich Milenin
Associate Professor, the Department of Surgery with the Traumatology-Orthopedics course, candidate of medical sciences, traumatologist-orthopedist
|
 |
Nikolay Vladimirovich Popov
Traumatologist-orthopedist
|
 |
Alisher Saydullayevich Hairullaev
Traumatologist-orthopedist
|
Contact Information
Address: 105203, Moscow, Nizhnyaya Pervomayskaya str., 70
Contact phone number:
Fax:
How to reach us by using public transport
“Pervomaiskaya” metro station (last carriage of the train out of the city centre). From “Pervomaiskaya” metro station by any tram or trolley bus go to the stop “15th Parkovaya Street”. Go along the 15th Park Street to the intersection with the Nizhnyaya Pervomaiskaya Street, turn left and walk about a hundred meters to the entrance of the Pirogov National Medical and Surgical Center.