The head of the clinic: Fayzrakhmanov Rinat Rustamovich, ophthalmologist of the highest category, Ph.D.
Ophthalmology center was established on July 1, 2003, and since December 26, 2016 has started work in a new, even more technologically advanced format — modern operating and diagnostic rooms have been opened, the latest equipment has been installed.
An important advantage of Ophthalmology center is its location on the basis of a multidisciplinary surgical center. Availability of a wide range of high-tech research and treatment activities, involving, if necessary, doctors of all specialties, allows diagnosing and treating patients in the presence of comorbidities.
Ophthalmology Center is the base for the Ophthalmology Department of the Institute for Advanced Training of Physicians of the National Pirogov Medical and Surgical Center
Thus, a comprehensive approach to the treatment of eye diseases of various etiologies is provided, the best clinical and functional results and the most complete medical, social and professional rehabilitation of patients with ophthalmic pathology are achieved.
Ophthalmology center provides:
- Inpatient examination and treatment for the following diseases:
- Outpatient examination and treatment for the following diseases:
- Inflammatory diseases of the eye
- Myopia, hyperopia, astigmatism, presbyopia
- Corneal Dystrophy
- Acute attack of closed-angle glaucoma
- Open-angle glaucoma
- Secondary cataract
- Tension syndrome in the anterior capsule of the lens after cataract surgery
- Proliferative diabetic retinopathy
- Retinal tear, local retinal detachments
- Dystrophy of the retina of different etiology and localization
- The consequences of acute circulatory disturbances in the central vein of the retina and central retinal artery
- Dry and wet types of age-related macular degeneration of the retina
- Proliferative diabetic retinopathy
- Intraocular hemorrhage
- Intraocular neoplasms
- Chalazion, cysts and neoplasms of the eyelids
- Pterygium and conjunctival cysts
In the Ophthalmology center we apply modern technologies of eye microsurgery, including in outpatient settings:
- Vitreoretinal surgery
- Combined organ-preserving surgery with intraocular melanomas
- Retinal Laser Surgery
- Ultrasonic cataract phacoemulsification
- Unique technologies for severe forms of eye diabetes, with the consequences of severe eye injury
- Corneal transplantation with the use of the technology of penetrating and lamellar keratoplasty
- Photorefractive operations using excimer laser technologies for myopia, hyperopia and astigmatism
- Laser vision correction using the Femto-Lasik method on the newest femtosecond laser
- Using of excimer laser technologies for medical and optic-reconstructive surgeries for various diseases of the cornea
- Proprietary technologies of microsurgical and laser operations
Diagnostic testing and equipment
Full ophthalmological examination, including special high-tech research methods:
- Fluorescent angiography of the anterior and posterior segments of the eye on the retinal camera
- Optical coherence tomography (OCT) of the macula, optic disc, anterior segment of the eye on the modern optical coherent tomograph of the latest generation
- Autorefractometry
- Keratotopography on corneal topographer with a sheimpflug technology
- Intraocular pressure measurement by contact and non-contact methods
- Visocontrastometry
- Computer perimetry
- Critical Flicker Frequency test
- A- and B-scan ocular ultrasound
We use the latest laser systems:
- FemtoLaser
- Microscan
- Excimer laser
- Diode laser with micropulse mode
- Shock-wave YAG laser
Proprietary technologies:
- The technology of sparing vitreoretinal surgery of the most severe forms of eye diabetes
- The technology of combined surgery of large intraocular melanomas
- The technology of large intraocular foreign bodies removal, based on sparing combined vitreoretinal surgery
- Proprietary technology of seamless transconjunctival vitreoretinal surgery with the tunnel sclerostome formation and the use of ports for the introduction of instruments
- The technology of organ-preserving surgery for stopping the progression of the eyeball subatrophy
- Vitreoretinal surgery in the Ophthalmology Center of the National Pirogov Medical and Surgical Center
- Features of vitreoretinal surgery in the treatment of patients with diabetic retinopathy
- Features of vitreoretinal surgery in the treatment of patients with exudative form of age related macular degeneration
- Features of vitreoretinal surgery in the treatment of patients with large intraocular melanomas
- Prospects for the development of vitreoretinal surgery
Advice to patients
It is recommended that when you visit an ophthalmologist for the first time, you should have epicrisis excerpts or extracts from medical records (outpatient cards), results of examinations or treatment in other medical institutions, if any.
Contact Information
Address: 105203, Moscow, Nizhnyaya Pervomayskaya str., 70
Contact phone number:
Fax:
How to reach us by using public transport
“Pervomaiskaya” metro station (last carriage of the train out of the city centre). From “Pervomaiskaya” metro station by any tram or trolley bus go to the stop “15th Parkovaya Street”. Go along the 15th Park Street to the intersection with the Nizhnyaya Pervomaiskaya Street, turn left and walk about a hundred meters to the entrance of the Pirogov National Medical and Surgical Center.
Eye Diseases
- Optic nerve atrophy
- Intraocular melanoma
- Ophthalmic manifestations of diabetes mellitus
- Glaucoma
- Vascular and dystrophic retinal pathology
- Cataract
- Strabismus
- Retinal detachments
- Pterygium
- The neovascular form of age-related macular degeneration (AMD)
Optic nerve atrophy
Optic nerve atrophy is the process of complete or partial destruction of the nerve fibers and replacement of their connective tissue.
Causes
Experts call heredity and congenital pathology among the causes of atrophy of the optic nerve, in addition, it can become a consequence of various diseases of the organ of vision — pathological processes in the optic nerve or retina (inflammations, trauma, edema, stasis, toxic damage, circulatory disorders, dystrophy, compression optic nerve, etc.), diseases of the nervous system or common diseases.
Symptoms
There are primary and secondary atrophy of the optic nerve, complete and progressive, partial and complete, as well as one-sided and bilateral forms of the disease.
The main symptom of this pathology is a deterioration in vision, which is almost impossible to correct. This symptom can manifest itself in different ways, depending on the type of atrophy. Progressive atrophy leads to a steady decline in vision due to the dying of the optic nerve, which can lead to complete blindness. This process proceeds either rapidly — for several days, or occurs gradually, within several months.
With partial atrophy, the process of vision deterioration stops at some stage and vision stabilizes. Thus, it is possible to isolate atrophy progressive and complete.
Visual disturbances in atrophy can be very diverse, including changing the visual fields (usually narrowing when “lateral vision” disappears), up to the development of “tunnel vision”, in which a person sees through a tube, namely, sees only objects , located directly in front of him. This condition is accompanied by the appearance of scotomas — dark spots on any of the fields of vision or by the appearance of color-perception disorder.
Diagnostic
Diagnosis of atrophy of the optic nerve, usually, does not cause difficulties. Its basis is the definition of acuity and visual fields (perimetry), as well as the study of color perception. Sometimes, to clarify the diagnosis, there is a need for an
Treatment
Atrophy of the optic nerve almost does not give in to treatment, after all the destroyed nerve fibers simply can not be restored. There is little hope of the effect of the therapy of fibers that are in the process of destruction, but so far have retained their vital functions. However, if this moment is missed, the sight of the diseased eye will be lost forever. It should be borne in mind that atrophy of the optic nerve is often not an independent disease, but develops as a consequence of certain pathological processes of the visual pathway. That is why, as a rule, its treatment begins with the elimination of causes of pathology. Drug treatment is aimed at eliminating swelling and inflammation of the optic nerve fibers, improving its trophism and blood circulation (nutrition), restoring the conduction of not completely destroyed nerve fibers.
Intraocular melanoma
Intraocular (uveal) melanoma (UM) is a high-grade tumor and belongs to the category of rare tumors. The peak incidence of UM is at the age of 55 years. With UM, both the iris and the ciliary body and the vascular membrane can be affected, so a differentiated approach is necessary in the diagnosis and treatment of this tumor. The presence of photopsy, deterioration of central vision and the presence of visual field defects is characteristic of melanoma of the choroid.
Diagnostic
- Ultrasound Biomicroscopy
- Optical coherence tomography
- Fluorescence angiography is suitable for differential diagnostics of malignant and benign neoplasms, clarifying the boundaries of the tumor.
- Computer and magnetic resonance imaging
Treatment
Currently, there are two main types of treatment: organ-preserving and radical (removal of the eyeball, or enucleation). When choosing tactics for patients with intraocular melanoma, a systematic approach should be used, taking into account the clinical parameters of the tumor and the state of antitumor resistance of the organism. To expand the indications for the use of light energy and local radiotherapy, as well as increase their therapeutic effectiveness, biological response modifiers are used to aggravate the state of tumor cells and activate the function of the antitumor resistance of the organism. Such biological response modifiers include cytokines (interferons, interleukins (IL), tumor necrosis factor, etc.), inclusion of which into the complex of organ-preserving treatment of UM (light coagulation and brachytherapy) allows to increase the effectiveness of treatment of intraocular tumors, as well as cytostatics that increase sensitivity of tumor cells to radio emission.
Ophthalmic manifestations of diabetes mellitus
Diabetic retinopathy (DR) — a specific lesion of the retina vessels is characteristic for insulin-dependent and insulin-independent diabetes, leading to a significant reduction in vision (right up to blindness).
The main causes of the disease are vascular changes (increased permeability and growth of newly formed retinal vessels).
Treatment of diabetic retinopathy is usually carried out by two specialists — an ophthalmologist and an endocrinologist. It includes both the use of systemic agents (insulin therapy, antioxidant, angioprotectants), and local treatment — eye drops and laser intervention.
Treatment
Since diabetic retinal lesion has a secondary character, the deciding moment is systemic management of the underlying disease — regular monitoring of blood sugar level, as well as blood pressure and kidney function.
The most widely used method for treating diabetic retinopathy and macular edema is laser therapy performed on an outpatient basis. The essence of this method is as follows:
- Destroy the hypoxic zones of the retina, which is the source of growth of newly formed vessels
- Increase direct oxygen supply to the retina from the choroid
- To perform thermal coagulation of newly formed vessels
Vitrectomy — surgical intervention is prescribed with extensive intraocular hemorrhage or a neglected form of proliferative retinopathy. Its essence consists in operative removal from the eye cavity, blood clots, turbid parts of the vitreous body, fibrovascular cords from the retina surface. In this case, aspiration (suction of fluid) of the vitreous body should be carried out at the maximum full scale. The posterior hyaloid membrane located between the vitreous body and the retina, which plays an important role in the progression of proliferative retinopathy, is removed (if possible).
Diabetic macular edema (DME) — accumulation of fluid and/or thickening of the retina in the area of the macula. DME can develop at any stage of diabetic retinopathy. Visual acuity can be reduced, especially if the central part of the macular zone (central fossa) is involved, and may remain high for a long time if the changes are more peripheral to the central fossa.
Macular edema is difficult to diagnose with direct ophthalmoscopy, because it does not provide the stereoscopic vision necessary to detect a thickening of the retina. To diagnose DME, the fundus is examined with an enlarged pupil stereoscopically (binocularly) with a slit lamp and lenses (contact and non-contact). Stereoscopic images of the fundus and optical coherence tomography are important additional methods of investigation for suspected DME. Fluorescent angiography is often used to determine the volume and treatment method- laser coagulation (focal or reticular) or vitreoretinal surgery.
Diabetic macular edema is treated with a timely laser coagulation of the retina and the introduction of drugs into the vitreous cavity (Lucentis, Ozurdex).
Glaucoma
The term “glaucoma” (anc.Greek — blue clouding of the eye) occurs back in 400 BC in the works of Hippocrates. However, modern ideas about this disease began to form only in the Middle Ages.
Today the concept of “glaucoma” unites a fairly large group of eye diseases, of different course and origin. Strange as it may seem, there is still no consensus on the causes of the onset of the disease. However, in the absence of treatment, the outcome of these, completely different ailments, one is the total atrophy of the optic nerve and the subsequent blindness.
For a healthy eye, there is a definite, constantly maintained pressure
Developing, glaucoma disrupts the circulation of this fluid, which, without the possibility of outflow, accumulates inside and the eye pressure begins to grow steadily.
Under the influence of colossal loads, the blood supply to the optic nerve is impaired. As a result, its atrophy occurs, after which the visual signals can no longer flow to the brain. The person begins to see worse, peripheral vision is disturbed (the zone of visibility is limited). The result is blindness.
Today, experts identify the following clinical forms of the disease: open angle glaucoma and closed-angle glaucoma.
According to statistics, over 90% of all cases of this disease are open-angle glaucoma. With this form of disease, the natural drainage system of the eye loses its physiological functions, as a result of which, intraocular pressure begins to gradually increase. Often, the open-angle form of glaucoma is characterized by an asymptomatic and almost invisible course of the disease. Since the narrowing of the field of view is very slow (the process can drag on for several years), the patient sometimes absolutely accidentally discovers that he sees only with one eye. In some cases, however, you can hear patient’s complaints about the periodically appearing “rainbow circles” when looking at bright light, “misting” and asthenopic complaints associated with the weakening of accommodation.
With angle-closure glaucoma, intraocular fluid may accumulate due to lack of access to the anatomical drainage system, since the iris closes the angle of the anterior chamber. As a result, an increase in intraocular pressure, which can provoke an acute glaucoma.
Diagnostic
- Investigation of the patient’s field of vision (computer perimeter)
- Measurement of refraction (the ability of the optics of the eye to refract light rays)
- Measurement of intraocular pressure
- Ultrasound of the eye
- Measuring the depth of the anterior chamber and the thickness of the lens
- Evaluation of the structure of the angle of the anterior chamber, through which the fluid outflows (gonioscopy)
This allows us to identify the initial manifestations of the disease, which occur even before the earliest changes in vision, in time to begin treatment and stop the developing pathological process.
Treatment
Drug medications (eye drops) in this case are aimed only at reducing intraocular pressure. These medicines are presented a lot and all of them have different effects.
Operations
Often, the use of drops and physiotherapy is not enough to normalize the pressure and stop the loss of vision. Nonpenetrating deep sclerectomy (NDSE) is an operative intervention that allows restoring the natural balance of eye fluid in the open-angle form of glaucoma.
Closed-angle forms are treated both by traditional operations, and by the method of clear lens removal, followed by implantation of the intraocular lens (if the size of the lens does not correspond to the size of the eye).
Vascular and dystrophic retinal pathology
Retinal dystrophy is a very broad concept that encompasses a large number of individual diseases that are self-sufficient or arise from other diseases. Retinal dystrophy is one of the reasons for the deterioration or complete loss of vision. This disease is typical for people at a young age, and for the elderly. Dystrophy of the retina can for a long time not manifest itself subjectively, but it leads to irreversible changes in the eye.
All the dystrophies of the retina are divided into hereditary and acquired, the latter are divided in turn into peripheral and central.
Peripheral dystrophies are accompanied by degenerative changes in the periphery of the retina that do not affect the macular area and is usually a complication of eye inflammation, eye injury or myopia.
Central retinal dystrophy is the degenerative changes that occur in the macular area (the place of the most clear vision). The most common diseases are macular degeneration and serous central retinopathy.
Diagnostic
- Perimetry and visometry
- Examination of the fundus
- Fluorescent angiography
- Ultrasound of the eye
Treatment
The most effective method of treatment is laser coagulation — it prevents the development of a serious complication of dystrophy — retinal detachment.
Cataract
Cataract — a disease in which the transparency of the lens deteriorates, which leads to a decrease in visual acuity. The lens of a healthy person is a transparent optical lens through which light rays are focused on the retina. Cataracts gradually replace water-soluble proteins, which provide transparency of the lens, water-insoluble proteins, which is accompanied by concomitant inflammation and lens edema. When the transparency of the lens is deteriorated, the image obtained on the retina becomes fuzzy and, as it were, blurred. Cataract of the eye is a chronic progressive disease, the opacity of the lens is irreversible.
There are congenital and acquired cataracts. Acquired cataracts can be the result of age-related changes (senile cataracts), trauma of the eye (traumatic cataract), exposure to radiation (radiation cataracts), and other internal diseases (secondary cataracts).
Cataract develops gradually and proceeds painlessly. The first symptoms of cataract are manifested in the form of flies, small blackouts in front of the eyes, doubling. Patients have difficulty in reading due to a decrease in the contrast of the text, but visual acuity, as a rule, remains unchanged. The initial stage of the disease, at which the described symptoms do not progress, can last from several to
Diagnostic
For detection of the disease, the standard methods are used (slit lamp research — biomicroscopy, determination of acuity and visual fields, measurement of intraocular pressure, ophthalmoscopy) and special (densitometry, ultrasound) methods of ophthalmological examination.
Treatment
In the initial stages of cataracts, drug therapy is prescribed: eye drops containing vitamins (PP, A, B, C), antioxidants, amino acids, cysteine, glutathione, ATP.
Surgical treatment is the only radical method of cataract treatment. During the operation, the lens damaged by the cataract is removed, and an artificial intraocular lens (IOL) is placed in its place. Currently, the main operations that are performed in cataracts are ultrasound phacoemulsification, extracapsular or intracapsular lens removal, followed by the installation of the IOL.
Strabismus
Strabismus is a pathology in which one or both eyes, when viewed directly alternately deviate to the side, that is, they look in different directions. Normally, the movements of both eyes are symmetrical when looking at an object, therefore, images perceived by the right and left eye in the cerebral cortex are joined into a single volumetric picture (so called binocular vision). When the strabismus takes place the combined eyes work is disturbed, and it becomes impossible to combine images into a single image. To compensate for the resulting visual impairment, the central nervous system “turns off” the image that comes from the mowing eye. With the passage of time, a prolonged shutdown from the vision process of the mowing eye can lead to the development of amblyopia.
Often, strabismus can be detected already with external examination of the patient. In children up to the year, strabismus, detected by external examination, may be not genuine due to the peculiarities of the structure of the orbit at this age. A patient suffering from strabismus can complain about increased eye fatigue, frequent headaches, dizziness, unilateral vision impairment.
Strabismus can be a congenital or acquired pathology. Depending on the nature of the deviation of the eye from the visual axis, could be distinguished:
- Convergent strabismus (a synonym for esotropia), in which the mowing eye deviates toward the bridge of the nose. Pathology usually appears at an early age. Often occurs with farsightedness of medium or high degree.
- Divergent strabismus (synonym for exotrophy), in which the mowing eye deviates towards the temple. The cause of this type of strabismus may be medium or high degree myopia, especially in early childhood in case of trauma, infectious diseases, fright.
- Vertical strabismus, in which the eye is mowed upward or downward.
- Atypical and combined strabismus are rare forms of the disease associated with genetic disorders (such as Down’s syndrome, Moebius syndrome, Cruson syndrome, etc.).
Strabismus diagnosis
For the diagnosis of strabismus and the establishment of the form of the disease, a physical examination (eye movements, visual acuity, medium transparency, pupil responsiveness), binocular vision tests are used.
Treatment
It is important in time to identify and begin treatment of strabismus as soon as possible, because the prognosis and the possibility of restoring vision depend on this. Treatment of strabismus should be comprehensive. Apply spectacle correction (or wearing contact lenses), hardware methods of treatment to eliminate amblyopia.
Measures to restore binocular vision, in some cases, surgical treatment is required. The operation itself is mainly a cosmetic procedure and after it is still necessary to conduct a course of hardware treatment.
Retinal detachments
The retina is the inner thin shell of the eyeball, the localization of which falls on the area between the choroid of the eye and the vitreous body. Its function is perception of visual information. In the retina there are no sensitive nerve endings, so its disease proceeds painlessly.
The retina and the vascular membrane are normally located tightly, adjoining each other. The pathological state, characterized by their separation, is called a retinal detachment. If a person with a retinal detachment does not immediately provide qualified medical care, this process will become irreversible and fraught with a complete loss of vision.
Depending on the reasons that caused this pathology, there are:
- Traumatic detachment resulting from a trauma
- Regmatogenic (Greek “rhegma” - rupture) detachment, which is a consequence of rupture of the retina of the eye
- Traction detachment, which is associated with the stretching of the reticular membrane, characteristic of patients with changes in the vitreous
- Exudative detachment arising from the appearance of neoplasms or inflammatory eye diseases
Diagnostics
A comprehensive examination, undertaken with suspicion of retinal detachment, includes:
- Definition of visual acuity
- Audit of the fundus (ophthalmoscopy)
- The analysis of visual fields (perimetry)
- Ultrasound scanning
- Biomicroscopic studies
Treatment
This pathology is treated only in an operative way, and requires immediate surgical intervention. The goal of the treatment is to limit the area of rupture and prevent further progression of detachment. For this, extrascleral interventions (ballooning and filling of the sclera at the site of the rupture) and endovitral interventions (vitrectomy with pumping out the subretinal fluid and further tamponade of the rupture site) are used.
Laser treatment methods can also be used, including preventive and restrictive laser coagulation of the retina.
Pterygium
Pterygium is a common disease of the conjunctiva of the eyeball, characterized by its proliferation on the cornea of the eye. The disease progresses with time. The histological prerequisite for the formation of the pterygium is the common origin of the conjunctiva and the cornea. Many people do not notice the development of a pathological disorder because of the small and initially barely noticeable size of the neoplasm. Sometimes the pterygium quickly grows and advances to the pupil, reducing the visual acuity of the person and leading to a significant cosmetic defect.
Symptoms of the pterygium
- A slight opacity of the periphery of the cornea, which is the first sign of the developing pterygium. At this stage, the patient has no complaints. There is only a mild cosmetic defect.
- Appearance of build-up on the cornea, which has an opaque consistency. Such a growth is rather noticeable and usually grows from the side of the nose.
- Foreign body sensation in a particular eye that arises because the pterygium begins to rise above the surface of the cornea, irritating the receptors of the nerve endings located on the inner side of the eyelid.
- Irresistible eye irritation. The reason for this is the absence of a tear film on the surface of the neoplasm, as well as the disruption of the formation of this film on a healthy area of the cornea. A lasting feeling of dryness in the eye.
- Gradual decrease in visual acuity. This symptom appears when the pterygium grows on the center of the cornea, as a result of which the passage of light into the eyeball is deteriorated.
- If the pterygium is inflamed, there is hyperemia of the eyeball, itching, swelling of the conjunctiva, increased lachrymation.
Diagnostic
This pathology is revealed easily, as the doctor sees it with the naked eye.
Slit microscopy (biomicroscopy) helps a specialist to consider the focus of the lesion in more detail. This method of diagnosis allows you to evaluate the shape of the pterygium, to inspect its surface, determine the degree of its adhesion to the cornea.
Treatment
The pterygium is treated surgically and conservatively.
If the neoplasm does not affect the pupil and does not cause serious inconvenience to the patient, this focus can be left. An operation is performed in this case solely at the patient’s request in order to eliminate the cosmetic defect. The patient is prescribed artificial tear preparations and anti-inflammatory therapy. After surgical removal, the use of anti-inflammatory and antibacterial drops and ointments is prescribed for several days.
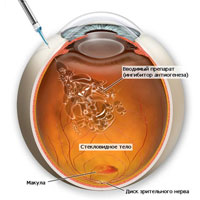
The neovascular form of age-related macular degeneration (AMD)
According to the World Health Organization, age-related macular degeneration is one of the most common causes of blindness and impaired vision in older people. Age-related macular degeneration is a chronic degenerative disorder, which most often affects people after 50 years. And, according to statistics, age-related macular degeneration is most often affected by women.
AMD is manifested by irreversible lesions of the macular zone with progressive deterioration of central vision. According to available data, the paired eye is affected no later than 5 years after the disease of the first.
In clinical practice two forms of AMD are distinguished: “dry” and “wet”. The “dry” form (9 out of 10 patients with AMD) is progressing for many years, causing a deep loss of central vision in only
With degenerative disorders, central vision decreases as a result of damage to the macula, the most important part of the retina.
Age-related macular degeneration in most cases leads to blindness and until today has been known as incurable disease. The methods that existed before allowed only to support the vision, but not to improve it.
Symptoms of a neovascular form of macular degeneration:
- Decreased visual acuity
- Reduced contrast sensitivity
- Central scotoma
- Metamorphopsy — the perception of objects in a distorted form
The goal of treatment of age-related macular degeneration
In the treatment of age-related macular degeneration, the goal is to prevent the growth of abnormal blood vessels by blocking growth stimulators of new vessels, as well as destroying the existing neovascular network in order to stop bleeding. To achieve this with the methods that existed before was not possible.
The real rescue was for the patients with age-related macular degeneration became the drug LUCENTIS, which in June 2006 was approved by the FDA as a unique tool for the treatment of age-related macular degeneration, and in 2008 — registered in Russia. Treatment with LUCENTIS allows not only to slow down the progressive decline in vision, but also to restore visual acuity in many patients.
The drug LUCENTIS is introduced into the vitreous humor at a dose of 0.5 mg (0.05 ml). First, 3 consecutive monthly injections of Lucentis (“stabilization” phase) are carried out, then the doctor recommends the number of injections depending on the state of visual functions and the degree of the disease (the phase of “maintenance”). The interval between doses is at least 1 month.
Injections of LUCENTIS are performed once a month (the course will be 3 injections). Usually after this comes the stabilization phase. However,
Peripheral dystrophies and retinal ruptures
In the detection of ruptures and thinning of the retina, treatment is carried out-prophylactic using laser coagulation of the retina or delimiting laser retinal coagulation. With the help of a special laser, the retina is exposed to the rupture edge, and thus the glue zone is “glued” to the underlying eye, which prevents the liquid from penetrating the retina and peeling it off at that place. Laser coagulation is carried out on an outpatient basis. It takes a few minutes and is well tolerated even by children. In some cases, for example, with insufficiently transparent eyes, cryopexy of the rupture zone (cold treatment) through the conjunctiva of the posterior wall of the eye is performed. This procedure can also be performed on an outpatient basis. Modern lasers make it possible to treat not only thinning and rupture, but also subclinical (i.e. small) and even flat limited retinal detachments.
Novus Spectra Ophthalmic Laser
Novus Spectra ophthalmic lasers are photocoagulators with improved optics, an extended range of capacities and unprecedented reliability.
The Novus Spectra dual-port system of ophthalmic laser is compatible with a wide range of accessories, which ensures optimal results both in the laser cabinet and in the operating room.
- Advantages of the Novus Spectra Ophthalmic Laser:
- Extended range of options
- DPSS (diode-pumped solid-state) technology of the latest generation allows the Novus Spectra compact system to adjust the radiation power from 50 to 2500 mW, and the active cooling system ensures a stable output of the laser beam.
- Ophthalmic lasers have excellent optics.
- Extended range of options
- Homogeneous laser beam
- Professional optics and an advanced laser beam delivery system ensure an even distribution of energy throughout the focal spot of the ophthalmic laser, making retinal manipulations unprecedentedly accurate and safe.
- As a result, we get a uniform laser spot with a uniform energy distribution throughout its area, which excludes the possibility of formation of “hot spots” in this area.
- ClearView filters
- Perfect visualization of the ophthalmic laser.
- Lumenis ClearView filters with a special coating eliminate color distortion and improve the transmission of white color. This coating protects the filter from scratches and the influence of damaging environmental factors.
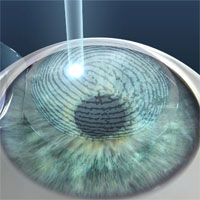
Laser vision correction
LASIK is the most popular method of laser vision correction in the world, according to which several million operations are performed every year. LASIK is the abbreviation of the full name of the operation “Laser Assisted In Situ Keratomileusis”, proposed by the Greek doctor Pallikaris back in 1990.
To date, LASIK is the safest, hi-tech and time-proven method of laser vision correction, which allows to obtain high visual acuity and stability of results. LASIK is used to correct myopia, hyperopia and astigmatism, allowing patients to get rid of glasses and contact lenses.
Why did this technique become so popular?
LASIK has a number of advantages over other refractive operations:
- Rapid recovery of vision
- Lack of pain
- Short operation time
- Absence of stitches and scars
- Stability of results
The essence of the LASIK method is the use of the “cold” ultraviolet light of the excimer laser to change the optical power of the cornea. The change in the refraction of the cornea makes it possible to achieve precise focusing of the light rays on the retina, which determines the high visual acuity. Patients with myopia have a too steep form of the cornea, and the goal of LASIK is to make it more flat. Patients with hyperopia, in contrast, need to give the cornea a steeper form. With astigmatism, the cornea is given a regular spherical shape.
Operation LASIK consists of 3 main stages:
- Creation of a corneal flap
- Laser correction
- Return of the corneal flap to its original position
The entire operation takes
The patient may be disturbed by lacrimation, bruising and a feeling of sand in the eyes. A bright light can enhance these sensations, so you need to protect your eyes with dark glasses. Day after surgery, you should avoid any contact with the eye so as not to dislodge the corneal flap. A prerequisite for a successful operation result is strict adherence to all limitations and prescriptions of the attending physician. The patient receives a detailed treatment regimen of
The next day after surgery, the patient comes for a follow-up visit. In most cases by this time, visual acuity is as close as possible to the predicted, but without glasses and contact lenses. The visual acuity may fluctuate and vary slightly within a few days or weeks while the active healing process is in progress, depending on the individual characteristics of the patient.
LASIK refers to cosmetic procedures, and in most clinics a sick leave sheet is not issued. The patient can start his work or study the very next day after the operation, if it does not contradict the restrictions.
Most people achieve 100% visual acuity after LASIK, and sometimes more. The main task of LASIK is to save the patient from wearing glasses and contact lenses.
In rare cases, after receiving a high visual acuity after the operation, patients can note a gradual deterioration of vision in the distant period, the so-called “regression”. This may be due to progressive myopia, when the eyeball continues to grow in length. This issue can be discussed with the surgeon to determine whether it is possible to carry out pre-correction with the help of a second LASIK.
Even if you have excellent eyesight after LASIK, by the age of 45 you may still need reading glasses. This is a normal physiological process, called presbyopia. Your vision in the distance will remain clear, but when working at close range you will experience difficulties.
Very often you can find the term “Super Lasik”. But in scientific medical publications this term “Super Lasik” (with the prefix “Super”) is not used. Manufacturers of laser equipment for correction of vision also do not use this term. The name “Super Lasik” has received some distribution in advertising of both Russian and foreign medical clinics, apparently trying to attract additional attention due to “bright terminology”.
Pan retinal laser photocoagulation (PRP)
The main goal of PRP in the treatment of retinopathy is to destroy all areas of the retina with impaired blood supply by the laser. Laser exposure to these areas leads to the fact that the retina ceases to produce vasoproliferative substances that stimulate neovascularization, causing regression of already existing newly formed vessels, thereby leading to stabilization of the proliferative process. With the timely detection of newly formed vessels, laser coagulation of the retina can prevent blindness in the vast majority of cases.
This method is used mainly in the proliferative form of diabetic retinopathy and in pre-proliferative diabetic retinopathy characterized by the presence of extensive areas of retinal ischemia with a tendency to further progression.
Depending on the stage of diabetic retinopathy, the form of maculopathy, your treatment can include, on average,
Laser treatment of diabetic retinopathy in cases with a rapidly progressive form of fibrovascular proliferation in Type I diabetes mellitus, in the presence of newly formed vessels of the optic nerve disk, rapid progression of the process on the other eye, or in the neovascularization of the anterior segment of the eye implies a more active, “aggressive” tactic and maximum volumes of coagulation. In such cases, it is possible to perform at least 1000 coagulates for the first session, followed by the addition of another 1000 coagulates for the second session, usually in a week.
Treatment of retinopathy in diabetes should necessarily include subsequent examinations of patients and, if necessary, additional laser treatment. As a rule, the first examination after the primary laser treatment (panretinal laser coagulation of the retina) should be carried out after 1 month. In the future, the frequency of examinations is determined individually, an average of 1 visit in 1 — 3 months, depending on the severity of the course of diabetic retinopathy.
Laser retina coagulation is effective in 59% —86% of cases, allow to stabilize the proliferative process and maintain vision for many years in the majority of patients suffering from diabetes mellitus, with the proviso that adequate correction of such systemic factors as hyperglycemia, hypertension, nephropathy, heart failure maintained.